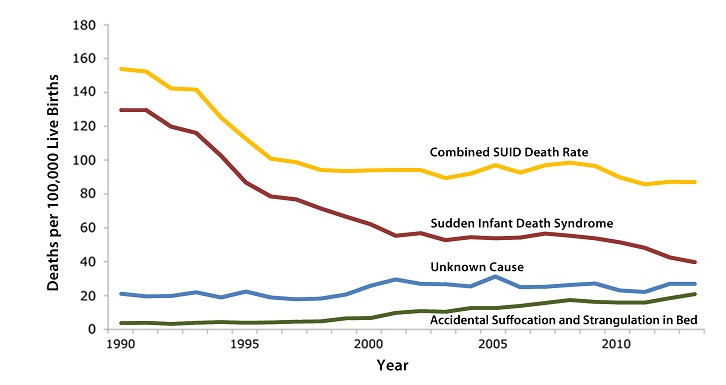
Statistics of SIDS incidences
SIDS in time
Overall statistics of SIDS incidences show that number of sudden deaths of infants declines. However, the biggest decrease we have seen in 90s – the result of the “Back to sleep” campaign. Since then, the decrease is much smaller, almost insignificant.
Sudden Infant Death Syndrome (SIDS) rates declined considerably from 130.3 deaths per 100,000 live births in 1990 to 55.7 deaths per 100,000 live births in 2001.
Unknown Cause infant mortality rates have remained unchanged from 1990 to 2010. In 2011, the Unknown Cause mortality rate in infants was 22 deaths per 100,000 live births.
Accidental Suffocation and Strangulation in Bed (ASSB) mortality rates remained unchanged until the late 1990s. Rates started to increase beginning in 1998 and reached the highest rate at 17.8 deaths per 100,000 live births in 2008.The total combined Sudden Unexpected Infant Death rate (which includes SIDS, Unknown Cause, and ASSB) declined considerably following the American Academy of Pediatrics safe sleep recommendations released in 1992 the initiation of the Back to Sleep campaign in 1994, and the release of the Sudden Unexplained Infant Death Investigation Reporting Form in 1996. However, the total combined Sudden Unexpected Infant Death rate has not decreased significantly since 1999.
SIDS per infant group
Sudden infant death syndrome happens from one every 200 births to one every 20000 births. There are several factors that increase the SIDS risk in certain groups of infants:
- Gestation age (data for US, in late 90s)
- at 37–39 weeks of gestation SIDS rate was 0.73/1000
- at 28–31 weeks of gestation SIDS rate was 2.39/1000
- Birth weight (related to gestation age, data for US, late 90s):
- for infants weighing 1000–1499 g SIDS rate was 2.89/1000
- for infants weighing 3500–3999 g SIDS rate was only 0.51/1000.
- Race/culture (see our explanation of genetics of SIDS, data for US, 2010-2013):
- for American Indian infants SIDS rate was 0.9/1000
- for Non-Hispanic Black infants SIDS rate was 0.8/1000
- for Non-Hispanic White infants SIDS rate was 0.4/1000
- for Hispanic infants SIDS rate was 0.3/1000
- for Asian/Pacific Islander infants SIDS rate was 0.2/1000
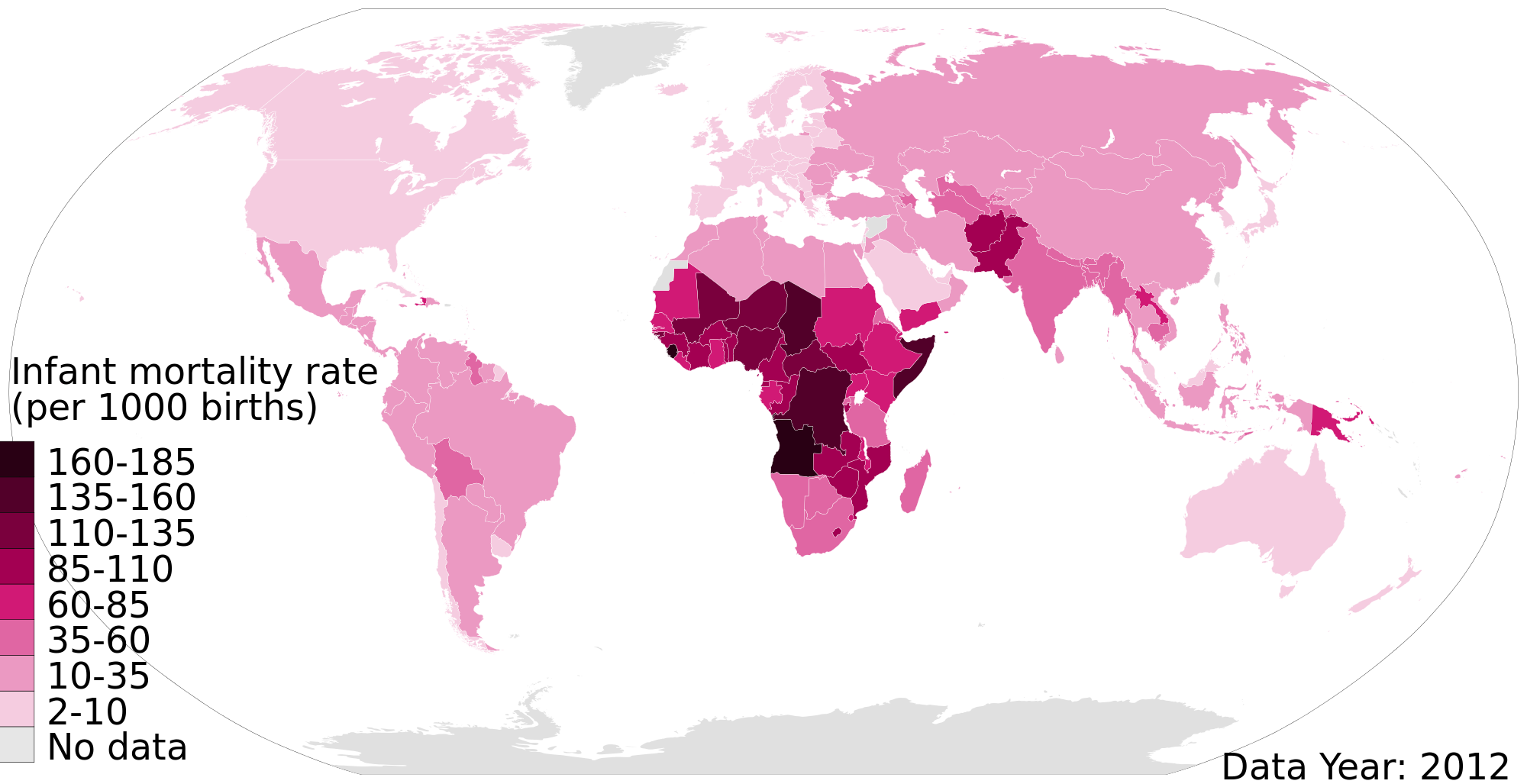
Comparing SIDS rates to infant mortality rates
Sudden infant death syndrome is not the only reason of infants’ deaths in the world. It is assumed that across the world, the leading causes of premature infant deaths were birth asphyxia, pneumonia, pre-term birth complications, neonatal infection, diarrhoea, malaria, measles and malnutrition. However, when only first world countries are taken into account, some research suggests SIDS is the third the most leading cause of infant mortality. Let’s compare the two rates in United Kingdom and United States:
- In UK overall SIDS rate is 0.2/1000, but it’s five times higher when mother is younger than 20. Infant mortality rate there is 4.19/1000, so SIDS is the cause of 5% of premature deaths of infants.
- In US overall SIDS rate (averaged across all groups) is 0.5/1000. Infant mortality rate is 5.97, so SIDS is the cause of 8% of premature deaths of infants.
The numbers are pretty similar and in both countries SIDS accounts for less than 10% of all premature deaths.